Pulse oximetry is a non-invasive method used to measure blood oxygen saturation (SpO2), a critical parameter in monitoring patients’ respiratory status. However, recent research and clinical observations have raised concerns about the accuracy of pulse oximeter readings across different skin tones. Understanding these effects is essential for healthcare providers to ensure accurate diagnosis and treatment.
How Pulse Oximeters Work
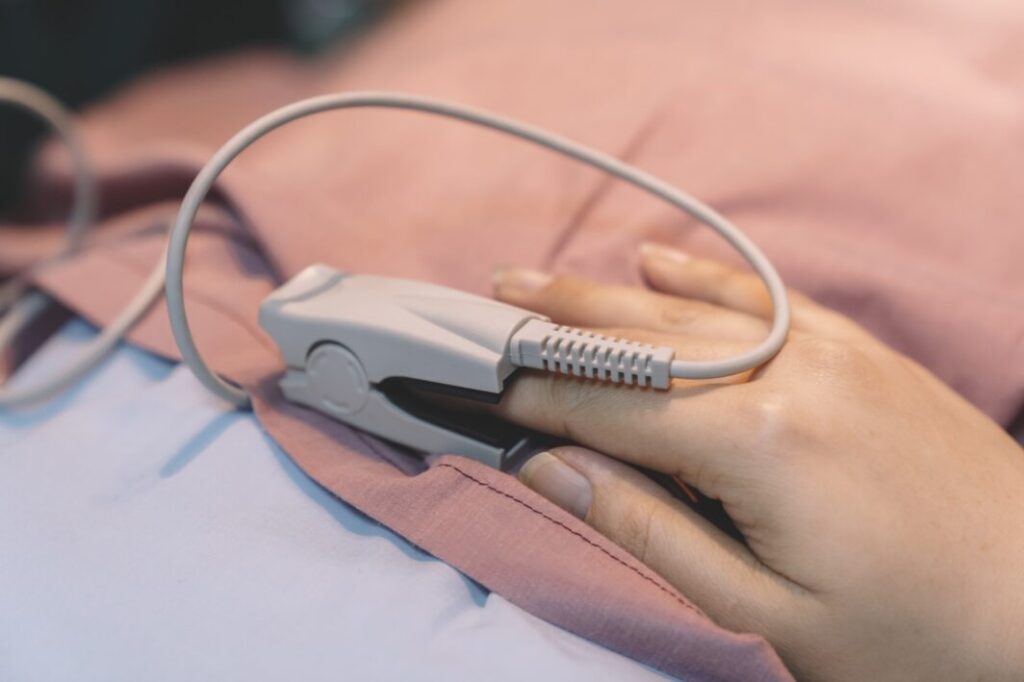
Pulse oximeters work by emitting light through the skin and measuring the absorption of light by oxygenated and deoxygenated hemoglobin. The device uses this information to calculate the oxygen saturation in the blood. Typically, a pulse oximeter probe is placed on a thin part of the patient’s body, such as a fingertip or earlobe.
The Influence of Skin Tone
Skin tone can influence the performance of pulse oximeters due to the varying levels of melanin, the pigment that gives skin its color. Melanin absorbs light, and higher levels of melanin in darker skin can interfere with the light absorption measurements that pulse oximeters rely on. This interference can lead to inaccuracies in SpO2 readings.
Research Findings
Several studies have demonstrated discrepancies in pulse oximeter readings between individuals with different skin tones. These studies have found that:
- Overestimation of SpO2: Pulse oximeters are more likely to overestimate oxygen saturation levels in individuals with darker skin tones. This overestimation can lead to a false sense of security in clinical settings, potentially delaying necessary medical interventions.
- Undetected Hypoxemia: The risk of undetected hypoxemia (low blood oxygen levels) is higher in patients with darker skin tones. This can be particularly dangerous in critical care settings, where timely detection and treatment of hypoxemia are crucial.
Implications for Clinical Practice
The potential for inaccurate pulse oximeter readings has significant implications for clinical practice. Healthcare providers need to be aware of these limitations and consider them when interpreting SpO2 readings. Here are some strategies to mitigate the effects of skin tone on pulse oximeter accuracy:
Supplemental Monitoring
In addition to pulse oximetry, using supplemental monitoring methods can provide a more comprehensive assessment of a patient’s oxygenation status. Arterial blood gas (ABG) analysis, which directly measures the levels of oxygen and carbon dioxide in the blood, can be used to confirm pulse oximeter readings and ensure accuracy.
Adjusting Clinical Thresholds
Healthcare providers may consider adjusting clinical thresholds for intervention based on the patient’s skin tone. For instance, maintaining a higher threshold for concern in patients with darker skin tones can help ensure that hypoxemia is not overlooked.
Device Calibration and Selection
Choosing pulse oximeters that have been validated for accuracy across a range of skin tones can help mitigate discrepancies. Some manufacturers are working on improving device calibration to account for skin tone variations. Using such devices can enhance the reliability of SpO2 readings in diverse patient populations.
Education and Training
Educating healthcare providers about the potential inaccuracies of pulse oximeters in patients with darker skin tones is crucial. Training programs should include information on the limitations of pulse oximetry and the importance of supplemental monitoring techniques. Awareness and education can empower healthcare providers to make more informed decisions and provide better patient care.
Patient Awareness
Informing patients about the limitations of pulse oximetry based on skin tone can also play a role in improving outcomes. Patients should be encouraged to communicate any symptoms of hypoxemia, such as shortness of breath or fatigue, even if their pulse oximeter readings appear normal.
Conclusion
The effects of skin tone on pulse oximeter readings highlight the need for greater awareness and improved practices in clinical settings. While pulse oximeters remain a valuable tool in monitoring oxygen saturation, understanding their limitations and implementing strategies to mitigate inaccuracies are essential steps toward equitable healthcare.
By incorporating supplemental monitoring methods, selecting properly calibrated devices, and educating both healthcare providers and patients, the medical community can work towards ensuring accurate and reliable SpO2 readings for all individuals, regardless of skin tone. Continued research and technological advancements will further enhance our ability to provide precise and effective care for diverse patient populations.