Anosmia, the loss of smell, and ageusia, the loss of taste, are rare side effects of many medications, particularly those affecting the cardiovascular system [1]. Anesthetic drugs are also implicated as catalysts for anosmia and ageusia; the incidence is estimated to be around 1.8% [2]. Although short-lived, these postoperative alterations in sensation can negatively impact patient quality of life. Patients with anosmia and/or ageusia are known to increase intake of sugar and salt, increasing the risk of chronic medical conditions such as diabetes, renal disease, or hypertension [3].
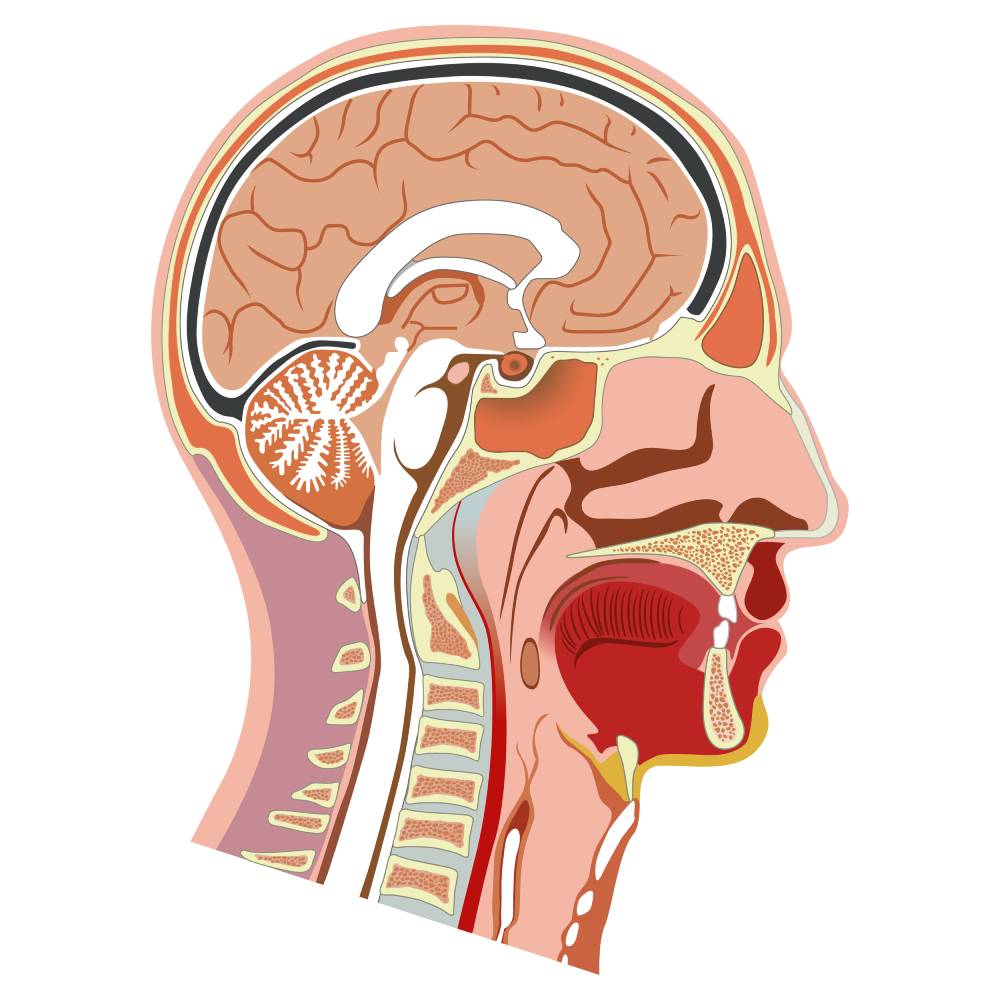
Known as the “chemical senses” because of their core characteristic of transmitting chemical stimuli as neural signals, the senses of smell and taste, or olfaction and gustation, are incredibly important in an individual’s perception of their environment. Odorant molecules are detected by olfactory receptors, which are G-protein coupled receptors found in the cilia of olfactory receptor neurons located at the top of the nasal cavity. The cell is then depolarized, which sends an action potential to the olfactory bulb, which then sends information up to the neocortex [4]. While there are only a limited number of olfactory neurons, each neuron can respond to multiple stimuli and each odor may stimulate multiple receptors, resulting in millions of possible neural combinations [5]. Unlike other neurons of the CNS, neurons of the olfactory and gustatory systems can replace themselves. Gustatory stimuli interact with gustatory receptor cells, which send signals to the brain via afferent nerve fibers in cranial nerves VII, IX, and X. Gustatory receptor cells are housed in taste buds, which collectively transmit information about 5 taste qualities: sweet, salty, sour, bitter, and umami. An ingested taste molecule will depolarize the corresponding taste cell, increasing intracellular calcium, leading to activation of afferent nerve fibers [4,6].
Most anesthetics activate GABA receptors in the CNS to elicit a sedative state; many of these receptors are found in taste and smell neurons. Decreased brain GABA has been noted in patients with phantogeusia and phantosmia (taste and smell hallucinations, respectively), clinical phenomena which are improved when GABAergic drugs are administered [7]. A research group in California found large doses of anesthetics depressed synaptic excitation of granule cells and prolonged post-synaptic inhibition of mitral cells in the olfactory tracts of animals [8]. Several case studies report long-lasting anosmia following surgery using anesthetics such as propofol, fentanyl, sevoflurane, ketamine, and others [7,9]. Mayell et al. also report a case of permanent anosmia after a chronic pain patient received intranasal ketamine [10]. Although each case is different, anosmia after anesthesia seems to be caused by alteration or destruction of olfactory receptor neurons; because these cells can generally replace themselves, it is not surprising most individuals will regain their sense of smell over time [5]. On the gustation side, the tongue is separated into two halves; the anterior two-thirds is innervated by the chorda tympani (a branch of the 7th cranial nerve) and the posterior part is innervated by the glossopharyngeal cranial nerve (the 9th cranial nerve) [11]. There is less data on changes in taste after anesthesia, but several case reports have described patients with full or partial loss of taste after procedures using general anesthesia. Whether the phenomena were due to anesthetic agents or other aspects of the procedure was not clear [5,7].
While postoperative alterations like anosmia or ageusia are not common, it can disrupt daily life and decrease patient satisfaction. Patients with postoperative alterations leading to lack of taste or smell may overcompensate by increasing the sweetness or saltiness of their diets, causing further complications. Anesthesiologists need to be aware of this possibility so that they are best equipped to prevent anosmia/ageusia or care for patients who have developed alterations in their chemical senses.
References
- Norès, J. M., Biacabe, B., & Bonfils, P. (2000). Olfactory Disorders due to Medications: Analysis and Review of the Literature. La Revue de medecine interne, 21(11), 972–977. https://doi.org/10.1016/s0248-8663(00)00253-8
- Kostopanagiotou, G., Kalimeris, K., Kesidis, K., Matsota, P., Dima, C., Economou, M., & Papageorgiou, C. (2011). Sevoflurane Impairs Post-operative Olfactory Memory but Preserves Olfactory Function: European Journal of Anaesthesiology, 28(1), 63–68. https://doi.org/10.1097/EJA.0b013e328340702b
- Green, T. L., McGregor, L. D., & King, K. M. (2008). Smell and Taste Dysfunction Following Minor Stroke: A case Report. Canadian Journal of Neuroscience Nursing, 30(2). https://pubmed.ncbi.nlm.nih.gov/18649778/
- Hadley, K., Orlandi, R. R., & Fong, K. J. (2004). Basic Anatomy and Physiology of Olfaction and Taste. Otolaryngologic Clinics of North America, 37(6), 1115–1126. https://doi.org/10.1016/j.otc.2004.06.009
- Elterman, K. G., Mallampati, S. R., Kaye, A. D., & Urman, R. D. (2014). Postoperative Alterations in Taste and Smell. Anesthesiology and Pain Medicine, 4(4). https://doi.org/10.5812/aapm.18527
- Yarmolinsky, D. A., Zuker, C. S., & Ryba, N. J. P. (2009). Common Sense about Taste: From Mammals to Insects. Cell, 139(2), 234–244. https://doi.org/10.1016/j.cell.2009.10.001
- Dhanani, N. M., & Jiang, Y. (2012). Anosmia and Hypogeusia as a Complication of General Anesthesia. Journal of Clinical Anesthesia, 24(3), 231–233. https://doi.org/10.1016/j.jclinane.2011.08.005
- Nicoll, R. A. (1972). The Effects of Anesthetics on Synaptic Excitation and Inhibition in the Olfactory Bulb. The Journal of Physiology, 223(3), 803–814. https://doi.org/10.1113/jphysiol.1972.sp009875
- Konstantinidis, I., Tsakiropoulou, E., Iakovou, I., Douvantzi, A., & Metaxas, S. (2009). Anosmia After General Anaesthesia: A case report. Anaesthesia, 64(12), 1367–1370. https://doi.org/10.1111/j.1365-2044.2009.06071.x
- Mayell, A., & Natusch, D. (2009). Anosmia—A Potential Complication of Intranasal Ketamine. Anaesthesia, 64(4), 457–458. https://doi.org/10.1111/j.1365-2044.2009.05911.x
- Lehman, C. D., Bartoshuk, L. M., Catalanotto, F. C., Kveton, J. F., & Lowlicht, R. A. (1995). Effect of Anesthesia of the Chorda Tympani Nerve on Taste Perception in Humans. Physiology & Behavior, 57(5), 943–951. https://doi.org/10.1016/0031-9384(95)91121-R