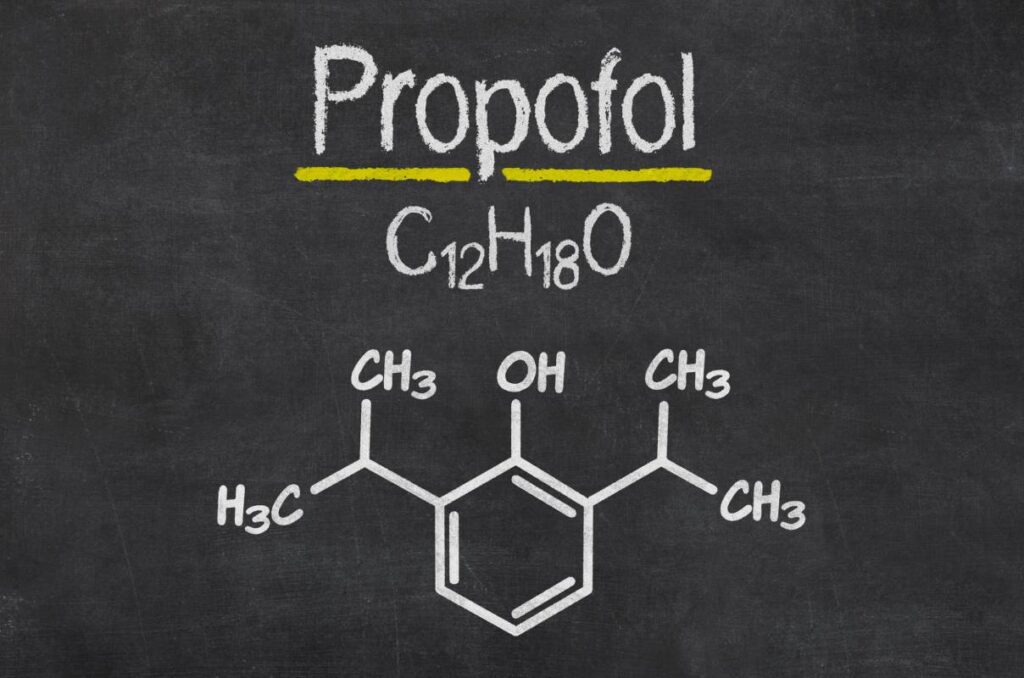
Propofol is a short acting sedative and hypnotic agent and the most widely used anesthetic in the world, due to having fewer post-anesthetic adverse effects compared to other anesthetic agents, such as ketamine or isoflurane [1]. The drug is also being used in neuroscience research to better understand consciousness and attention. One clinical study stressed the importance of the parietal and temporal lobes, suggesting the breakdown in connectivity between these regions caused by propofol is the neural correlate of decreased consciousness [2]. Propofol has long been considered to be dominantly GABAergic, but recent research suggests other molecular targets are involved. It is necessary for anesthesia providers to understand the pharmacology of propofol in order to optimize the anesthesia regimen and patient outcomes.
In the past, pharmology research identified propofol as an allosteric agonist for pentametric ligand-gated ion channels (pLGICs), particularly GABAA receptors [3]. Cl- channel formation is caused by activation of the β1 subunit, phylogenetically the oldest of the GABAA receptor subunits [4]. The bacterial homologue from Gloeobacter violaceus (GLIC), which is sensitive to anesthetic agents, forms a van der Waals connection with propofol molecules in the upper part of the transmembrane domain of each protomer [5]. This intra-subunit transmembrane cavity is most likely the binding site responsible for anesthesia’s inhibition of pLGICs. Propofol, etomidate, and halothane all bind to intra-subunit sites in nicotinic acetylcholine receptors (nAChRs), which are also inhibited by general anesthetics [5-8].
A homomeric pLGIC, such as GLIC, has five identical subunits and thus five equivalent binding sites for each receptor; a crystallization structural image shows five propofol molecules will bind symmetrically in each transmembrane domain [5,9]. This symmetrical (five-site) occupancy is thought to be standard for propofol-induced pLGIC inhibition. However, molecular stimulations demonstrated that asymmetrical binding to one, two, or three subunit sites accelerated channel dehydration, producing greater variance in the propofol-binding cavity size and imposing an unbalanced force which expedites channel conformation transitions [10]. Similarly, occupancy from one to three sites is enough to enhance receptor efficiency, indicating the channel is still functional [11]. Therefore, maximal functionality may be produced by asymmetrical, and not symmetrical, propofol binding [9].
An in vitro study found propofol may bind to the S4-S5 linker in KV1.2, a potassium channel, in a way that is functionally ineffective, which would explain why potassium channels are resistant to propofol [12,13]. On the other hand, sodium channels are inhibited by propofol, as demonstrated by a murine model [14]. While the precise mechanisms remain to be discovered, evidence for propofol-binding sites on these VGICs and others exists [9].
Kinesin is often likened to a locomotive running along microtubule “tracks” to assist cells in transporting different kinds of cellular cargo [9]. In single molecule experiments, clinically relevant concentrations of propofol reduced kinesin run length by 50% and decreased kinesin motility but had no effect on velocity [15]. This run length change is significant, since, for processive kinesins, each 8-nm step is equivalent to one ATP turnover [15]. This change might be a result of the excessive tubulin binding of propofol or effects within the kinesins themselves. Regardless, cellular cargo transported by affected kinesins arrives at its destination slower or not at all [9,15].
An immense amount of research has been done to better understand the role of propofol on its canonical molecular target, the GABAA receptor, but recent research has identified other molecular targets, such as pLGICs and VGICs, that play a role in its pharmacology. Propofol still has more unidentified molecular targets, which should incentivize further pharmacology research. Evidence suggests research into propofol’s interactions with its targets may even explain some of the drug’s adverse effects; for example, propofol’s effect on kinesins may be responsible for propofol-associated neurotoxicity [16].
References
- Lee, S. (2013). Guilty, or Not Guilty?: A Short Story of Propofol Abuse. Korean Journal of Anesthesiology, 65(5), 377–378. https://doi.org/10.4097/kjae.2013.65.5.377
- Schrouff, J., Perlbarg, V., Boly, M., Marrelec, G., Boveroux, P., Vanhaudenhuyse, A., Bruno, M.-A., Laureys, S., Phillips, C., Pélégrini-Issac, M., Maquet, P., & Benali, H. (2011). Brain Functional Integration Decreases During Propofol-induced Loss of Consciousness. NeuroImage, 57(1), 198–205. https://doi.org/10.1016/j.neuroimage.2011.04.020
- Forman, S. A., & Miller, K. W. (2011). Anesthetic sites and Allosteric Mechanisms of Action on Cys-loop Ligand-gated Ion Channels. Canadian Journal of Anesthesia/Journal Canadien d’anesthésie, 58(2), 191–205. https://doi.org/10.1007/s12630-010-9419-9
- Sanna, E., Garau, F., & Harris, R. A. (1995). Novel Properties of Homomeric β1 Gamma-aminobutyric acid type A Receptors: Actions of the Anesthetics Propofol and Pentobarbital. Molecular Pharmacology, 47(2), 213–217.
- Nury, H., Van Renterghem, C., Weng, Y., Tran, A., Baaden, M., Dufresne, V., Changeux, J.-P., Sonner, J. M., Delarue, M., & Corringer, P.-J. (2011). X-ray Structures of General Anesthetics bound to a Pentameric Ligand-gated Ion Channel. Nature, 469(7330), 428–431. https://doi.org/10.1038/nature09647
- Jayakar, S. S., Dailey, W. P., Eckenhoff, R. G., & Cohen, J. B. (2013). Identification of Propofol Binding sites in a Nicotinic Acetylcholine Receptor with a Photoreactive Propofol Analog. The Journal of Biological Chemistry, 288(9), 6178–6189. https://doi.org/10.1074/jbc.M112.435909
- Chiara, D. C., Hong, F. H., Arevalo, E., Husain, S. S., Miller, K. W., Forman, S. A., & Cohen, J. B. (2009). Time-resolved Photolabeling of the Nicotinic Acetylcholine Receptor by [3H]Azietomidate, an Open-state Inhibitor. Molecular Pharmacology, 75(5), 1084–1095. https://doi.org/10.1124/mol.108.054353
- Chiara, D. C., Dangott, L. J., Eckenhoff, R. G., & Cohen, J. B. (2003). Identification of Nicotinic Acetylcholine Receptor Amino acids Photo-labeled by the Volatile Anesthetic Halothane. Biochemistry, 42(46), 13457–13467. https://doi.org/10.1021/bi0351561
- Tang, P., & Eckenhoff, R. (2018). Recent progress on the Molecular Pharmacology of Propofol. F1000Research, 7, 123. https://doi.org/10.12688/f1000research.12502.1
- Mowrey, D., Cheng, M. H., Liu, L. T., Willenbring, D., Lu, X., Wymore, T., Xu, Y., & Tang, P. (2013). Asymmetric Ligand Binding Facilitates Conformational Transitions in Pentameric Ligand-gated Ion Channels. Journal of the American Chemical Society, 135(6), 2172–2180. https://doi.org/10.1021/ja307275v
- Roberts, M. T., Phelan, R., Erlichman, B. S., Pillai, R. N., Ma, L., Lopreato, G. F., & Mihic, S. J. (2006). Occupancy of a Single Anesthetic Binding Pocket is Sufficient to Enhance Glycine Receptor Function. The Journal of Biological Chemistry, 281(6), 3305–3311. https://doi.org/10.1074/jbc.M502000200
- Bu, W., Liang, Q., Zhi, L., Maciunas, L., Loll, P. J., Eckenhoff, R. G., & Covarrubias, M. (2018). Sites and Functional Consequence of Alkylphenol Anesthetic Binding to Kv1.2 Channels. Molecular Neurobiology, 55(2), 1692–1702. https://doi.org/10.1007/s12035-017-0437-2
- Kalstrup, T., & Blunck, R. (2018). S4–S5 Linker Movement during Activation and Inactivation in Voltage-gated K + Channels. Proceedings of the National Academy of Sciences, 115(29). https://doi.org/10.1073/pnas.1719105115
- Ouyang, W., Wang, G., & Hemmings, H. C. (2003). Isoflurane and Propofol inhibit Voltage-gated Sodium Channels in Isolated rat Neurohypophysial Nerve Terminals. Molecular Pharmacology, 64(2), 373–381. https://doi.org/10.1124/mol.64.2.373
- Bensel, B. M., Guzik-Lendrum, S., Masucci, E. M., Woll, K. A., Eckenhoff, R. G., & Gilbert, S. P. (2017). Common General Anesthetic Propofol Impairs Kinesin Processivity. Proceedings of the National Academy of Sciences, 114(21). https://doi.org/10.1073/pnas.1701482114
- Eckenhoff R.G., Jevtovic-Todorovic V. Chapter 15 Perioperative and Anesthesia Neurotoxicity. Miller’s Anesthesia Edited by Miller R.D., Cohen, N.H., Eriksson, L.I., Fleisher, L.A., Weiner-Kronish, J.P., Young, W.L. Philadelphia, Elsevier, 2015; 329–346.